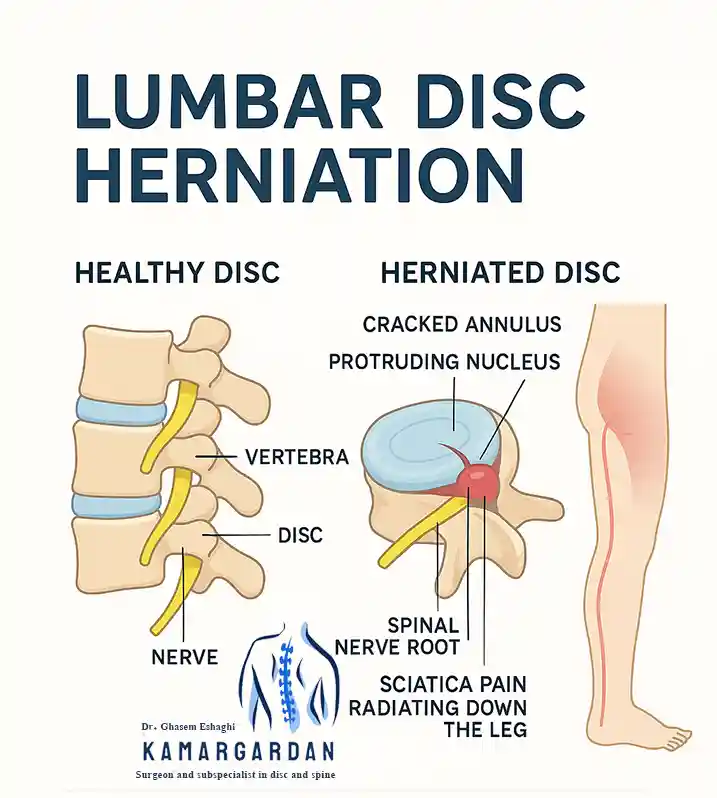
The lumbar disc is like a ball bearing — the nucleus rotates inside the annulus of the disc, and the annulus itself is attached to the vertebrae. This living “ball bearing” allows the movements of the spine. In one of these movements, the annulus of the disc may crack, which is commonly referred to as a degenerated (worn-out) disc. In another movement, the fissure in the annulus may enlarge, causing the contents of the disc to protrude outside the annulus and press on a nerve. The exact cause of lumbar disc herniation is unknown. Genetic predisposition is considered the most important factor. In other words, people who suffer from disc herniation often have discs of poor quality, and otherwise, even heavy physical work would not necessarily cause a rupture.
Treatment of Lumbar Disc Herniation
Despite the development of minimally invasive techniques, surgery is still considered the best treatment for lumbar disc herniation.
Reasons why surgery remains the best treatment for lumbar disc herniation:
- During surgery, the ruptured portion of the disc is removed, allowing the annulus to heal and fuse, preventing future leakage.
- The compressed nerve root is directly visualized, and the pressure is relieved.
- The recurrence rate is low; about 4% of discs relapse after surgery.
Surgical Methods for Treating Lumbar Disc Herniation
- Microsurgical discectomy (Laminectomy): A common method for removing the herniated disc material under a microscope.
- Minimally invasive endoscopic surgery: Allows the patient to return to work sooner without the need for large incisions or tissue removal.
- Laser disc decompression (PLDD): Performed for bulging or degenerated discs, using laser energy to reduce disc volume and pressure.
Non-invasive treatments for disc rupture include physical therapy and anti-inflammatory drugs, commonly referred to as painkillers by the general public.
Herbal Treatments for Lumbar Disc Herniation
The first remedy modern humans discovered for disc rupture was herbal medicine. The first anti-inflammatory drug created by humans was derived from willow bark — known as aspirin.
Other herbal-based remedies include:
- Piascledine: Extracted from avocado fruit.
- Curcumin: Derived from turmeric, available in 40 mg and 80 mg capsules.
- Devil’s claw extract (Doloteffin): Used in various herbal preparations for joint and back pain.
Causes of Lumbar Disc Herniation
- Genetic predisposition:
- Multiple genes are involved in disc rupture. It is estimated that about 75% of cases have a hereditary origin.
- Dehydration:
- Dehydration of the body and lumbar disc leads to degeneration. A recent study examining discs removed from 18 patients who underwent surgery for L4–5 or L5–S1 herniations found that Aquaporin-I levels correlated with MRI signs of disc dehydration.
- Mechanical overload on the spine:
- Not all herniations occur in degenerated discs. Some patients have herniations without significant degeneration or loss of water content. Static and dynamic overload — such as prolonged sitting or repetitive forward/backward bending — can increase the risk, especially in younger sedentary individuals.
- Inflammatory signals:
- Infection with Propionibacterium acnes, acidic environment formation, and microstructural changes in the nerve root can trigger inflammation.
- Factors like COX-2, FSTL1, and TNF-α have been shown to be significantly higher locally and systemically in patients with lumbar disc herniation compared to controls.
Symptoms of Lumbar Disc Herniation
Lumbar disc herniation is a general term that covers various types, similar to how the word “person” can refer to many different kinds of individuals.
Does a disc behave like a living being?
Yes. Unlike a pebble that passively presses on a nerve root, the disc is living tissue and can behave differently over time.
Possible locations of disc rupture:
- Midline
- Right side
- Left side
- Inside the intervertebral foramen
Key symptoms include:
- Low back pain: Caused by irritation of pain-sensitive fibers before nerve compression occurs.
- Sciatica: Pain radiating along the sciatic nerve from the back down to the buttock, thigh, and calf. It may be unilateral or bilateral.
Some patients have only leg pain without back pain, especially if the rupture is peripheral rather than central.
Severe cases:
A large herniation can compress all nerve roots in the spinal canal, causing sudden leg paralysis and urinary/fecal incontinence or retention.
Other possible neurological signs:
- Foot drop (difficulty lifting the front of the foot)
- Recurrent ankle sprains due to weakness
- Knee giving way (due to L3–L4 root involvement)
- Numbness, tingling, or “pins and needles” sensations
- Abnormal hot or cold sensations in the legs
The severity of symptoms is not always proportional to the size of the herniation — a small but high-pressure disc can cause more pain than a large, low-pressure one. Some ruptures are asymptomatic, especially if the spinal canal is wide and internal disc pressure is low.
Can a Herniated Disc Heal Naturally?
Yes. Healing is similar to a skin wound — small tears may heal with rest, but larger ones (especially in high-motion areas) may require “stitches” (surgery).
Healing process requires:
- Removal of extruded nucleus material between annulus edges.
- Reduction of internal disc pressure to bring edges closer.
- Growth of collagen tissue to close the annular tear.
- Time (about one month) for collagen to strengthen.
The body naturally:
- Sends macrophages to remove the extruded fragment.
- Reduces activity due to pain, lowering disc pressure.
- Initiates collagen repair.
About 80% of ruptures heal without surgery.
Why Some Herniated Discs Don’t Heal and Need Surgery
About 20% require surgery because:
- The extrusion is too large for macrophages to remove.
- Disc pressure remains high.
- Immune or collagen production is weak.
What Happens After Surgery
The surgeon replicates the natural healing steps:
- Removes part of the nucleus to reduce pressure.
- Stabilises unstable vertebrae with pedicle screws if necessary.
- Allows collagen tissue to close the annular tear.
Why Some Discs Re-Rupture
Patients who recover may forget they had a herniation and lift heavy loads or make sudden movements, raising disc pressure and tearing the weaker scar tissue.
Frequently Asked Questions :
1. What is lumbar disc herniation?
Lumbar disc herniation occurs when the inner nucleus of the spinal disc protrudes through a tear in the annulus, pressing on nearby nerves and causing pain.
2. What are the main causes of lumbar disc herniation?
The main causes include genetic predisposition, disc dehydration, mechanical overload (such as prolonged sitting or heavy lifting), and inflammatory processes.
3. What are the common symptoms of a herniated lumbar disc?
Symptoms include low back pain, sciatica, leg numbness or tingling, muscle weakness, foot drop, and in severe cases, paralysis or bladder/bowel issues.
4. How is lumbar disc herniation treated?
Treatment options range from physical therapy, pain medication, and herbal remedies to advanced surgical methods such as microsurgical discectomy, endoscopic surgery, and laser decompression.
5. Can a lumbar disc herniation heal without surgery?
Yes, about 80% of cases heal naturally with rest, reduced disc pressure, and collagen repair, but around 20% require surgery if the extrusion is too large or healing is incomplete.
Conclusion
Lumbar disc herniation is a common yet treatable condition. In about 80% of cases, healing occurs naturally through rest, reduced disc pressure, and the body’s repair mechanisms. However, in around 20% of patients, the severity of the herniation or insufficient healing makes surgery necessary. Fortunately, today various options such as microsurgical discectomy, endoscopic surgery, and laser disc decompression, along with non-surgical approaches like physical therapy and herbal medicine, provide patients with a wide range of effective treatment choices. The appropriate method should always be determined based on each patient’s condition under the supervision of a specialist.
Among these specialists, Dr. Ghasem Eshaghi stands out as an experienced spine surgeon, well-known for applying modern and minimally invasive techniques in the treatment of lumbar disc herniation. His expertise and careful selection of the most suitable treatment for each patient have helped many individuals achieve recovery with minimal complications and faster rehabilitation.